For the past century, antibiotics have been a cornerstone of medicine. Theyʼve made deadly diseases survivable, saved limbs from amputation, and made possible now-ubiquitous treatments like chemotherapy, organ transplants, and open-heart surgery.
Itʼs almost impossible to imagine a world where these drugs are not available to halt growth of bacteria and save lives, a world where infections like pneumonia and sepsis can once again be a death sentence.
But that reality is inching back into view.
Over 1 million deaths per year are attributable to bacterial antimicrobial resistance. By 2050, the WHO predicts that number will reach almost 2 million per year—a grim reminder that the future of antibiotics is a far cry from its “miracle drug” origins.
In the fall of 1928, Alexander Fleming returned from a holiday to his lab at St. Mary’s Hospital in London, where he was conducting experiments with staphylococcal bacteria. In an uncovered culture by an open window, he noticed mold colonies growing that seemed to be killing off the surrounding bacteria. He later determined it wasn’t the mold—a strain of Penicillium—but a “juice” it produced that killed the bacteria. He dubbed the substance penicillin.
In his petri dishes, Fleming found that penicillin could knock out the bacteria that cause diseases like scarlet fever, pneumonia, gonorrhea, meningitis, and diphtheria. But he struggled to isolate and purify the drug for clinical use.
A decade after his discovery, a team of Oxford researchers did just that, conducting experiments in mice and then, in 1941, on a British police officer covered with abscesses. The drug was astonishingly effective in just 24 hours—but the small amount of available penicillin ran out before the infection was fully treated, and the officer died a few weeks later.
Penicillin remained in short supply—so short that it was sometimes extracted from patientsʼ urine to be reused.
That changed later in 1941 when the Oxford scientists traveled to the U.S., where government scientists led a wartime effort, alongside pharmaceutical companies, to scale the drug, ultimately developing a fermentation method that dramatically expanded production.
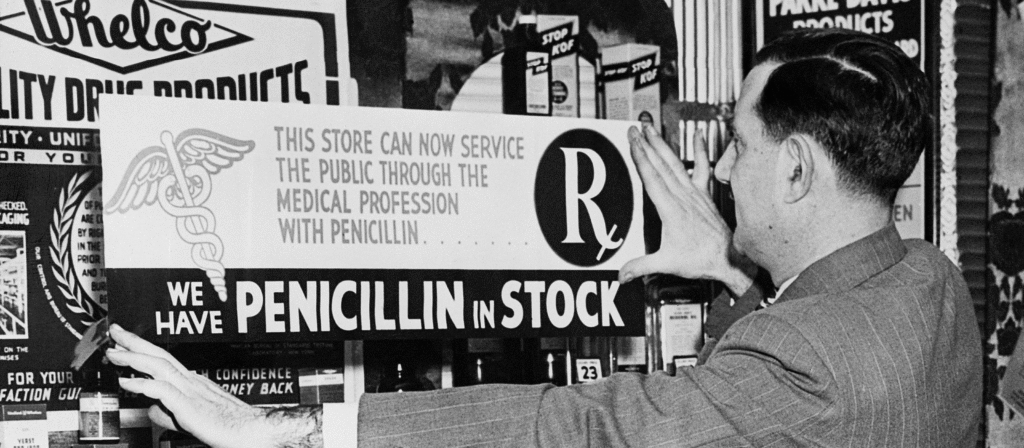
In the late 1940s, the nascent UN and WHO pledged to spur penicillin’s global production and distribution, funding equipment and training around the world. At the same time, the drug’s growing availability spurred its overuse and misuse, an issue Fleming had anticipated.
Accepting the Nobel Prize for his discovery in 1945, he warned that “the time may come when penicillin can be bought by anyone in the shops.” He gave the example of a hypothetical Mr. X, who had a sore throat and used enough penicillin to “educate” the Streptococci to resist the drug, but not enough to kill the infection. He then passed it on to his hypothetical wife, who died from the drug-resistant infection.
“Moral: If you use penicillin, use enough,” he said.
The warning went unheeded. Penicillin became widely available in a plethora of forms. It even turned up in cosmetic creams.
But it was the golden age of antibiotic discovery, and dozens of new antibiotics emerged from the 1940s through the 1960s, including methicillin, streptomycin, chloramphenicol, erythromycin, and vancomycin. “Clinicians and patients thought that we would always be a step ahead” of the bacteria, says Scott Podolsky, MD, director of the Center for the History of Medicine at Harvardʼs Countway Library.
For a while that was true. The development of novel antibiotics largely kept pace with demand. Pharmaceutical giants were excited by antibioticsʼ promise and made significant R&D investments to get them to market.
In 1961, the first reports of methicillin-resistant Staphylococcus aureus emerged, followed in 1967 by penicillin-resistant S. pneumoniae. The list has grown over the decades.
Flemingʼs warning had been a “truly a prophetic statement, and one which we are still grappling with,” says Anthony So, MD, MPA, distinguished professor of the practice in International Health.
By the end of the 1970s, pharmaceutical companiesʼ interest in antibiotics had already dwindled. In the 1980s, as Big Pharma pursued more lucrative drugs for cancers and chronic conditions, the search for novel antibiotics was left to smaller firms that were, and still are, frequently bankrupted by efforts to bring new antibiotics to market.
By the new millennium, “there was concern that we weren’t going to win this arms race,” says Podolsky. Still, resistance continued to rise as momentum dwindled.
Today, absent a flurry of new drugs, stemming the global tide of antibiotic resistance requires solutions that lie not in the drugs themselves, but in finding ways to use less of them. These include educating health workers in best prescription practices (one in four antibiotics prescribed in outpatient settings are unnecessary), reducing the need for antibiotics by improving hygiene and sanitation in global health, and vaccinating children.
As for the drugs themselves, their value must be measured not in sales volume, but in their value to society, says So.
“If you sell more antibiotics, you drive more resistance,” he says. “Unless you de-link that tie, you cannot actually get a business model that works. We can pay more now to address antimicrobial resistance, or pay much more later.”